It’s Crohn’s & Colitis Awareness Month – May 2021!
Inflammatory bowel disease is a collective term used for the diagnosis of Crohn’s disease, ulcerative colitis, or colitis in another form. These diseases are life-long autoimmune conditions, affecting people of all ages.
Approximately 85,000 Australians are living with Inflammatory Bowel Disease (IBD). In the month of May, Club Active are taking a closer look at Crohn’s and Colitis, to raise awareness on Inflammatory Bowel Disease and how someone can best manage it.
The statistics
- Inflammatory Bowel Disease affects 1 in every 250, with most diagnoses occurring between the ages of 15-35.
- It is estimated that 20-25% of people suffering from Inflammatory Bowel Disease will have a first-degree relative (first cousin or closer) with the disease.
- Inflammatory Bowel Disease impacts both men and women equally and affect most populations.
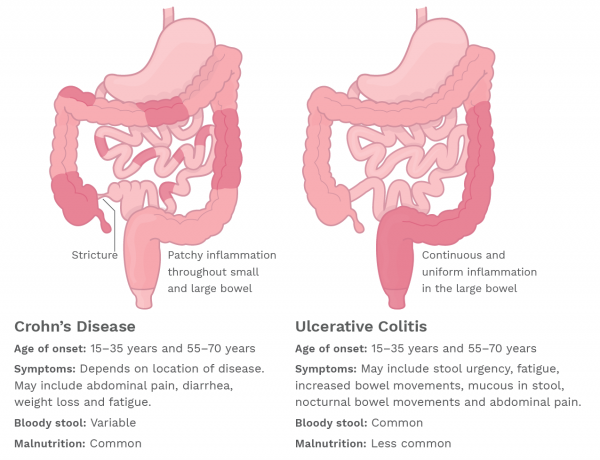
What is the difference between Crohn’s and Colitis?
Crohn’s disease and colitis have similar symptoms, however, each disease effects different parts of the gut.
Crohn’s disease
Can impact any part of the gastrointestinal tract (GI), ranging from the mouth to the anus. Inflammation caused by Crohn’s disease can involve different areas of the digestive tract and can cause inflammation spread through the entire thickness of the bowel wall. Crohn’s disease symptoms vary depending on which part of the gut is affected.
Colitis
Most commonly ulcerative colitis affects the large intestine, which is important for absorbing water and storing stools. This inflammation is often detected in the colon and at the rectum and only affects the innermost lining of the gut. There are many different forms of colitis depending on which region of the colon it affects.
What causes Crohn’s and Colitis?
No clear cause of Inflammatory Bowel Disease has been found. Researchers suggest that there are a number of factors occurring at the same time, that could trigger the initiation:
- Genetic predisposition makes a person more susceptible to developing the disease as well as;
- An encounter with an environmental trigger such as bacteria, a virus, or protein.
This can cause the immune system to respond and defend the body against the foreign substance, leading to inflammation. In most cases, once the substance has been destroyed the immune system turns off, but in people with Inflammatory Bowel Disease, the inflammation continues and causes damage to the intestinal tract.
Signs and Symptoms
- Abdominal pain
- Diarrhoea
- Bloody stools/rectal bleeding
- Weight loss
- Fatigue
- Anaemia
- Altered Appetite
- Ulcers in the gut
- Ulcers in the mouth
How is it managed?
Those diagnosed with Inflammatory Bowel Disease can experience times where it is actively known as a flare or in remission (inactive). The goal for people with this disease is to stay in remission and reduce flare ups and to make sure that the body gets enough nutrition to stay healthy. In some severe cases, surgery may be required to remove damaged parts of the gut. In cases of acute malnutrition, enteral nutrition may be required to received adequate nutrition.
- Regular check-ups with your doctor to help manage your symptoms and;
- Routine visits to a dietitian will help ensure that you are getting the right nutrition to fuel your body, especially as your nutritional needs may change during periods of flares and remission.
What should I eat during a flare up?
Your gut may not be able to absorb nutrients effectively therefore it is important to:
- Aim for small frequent meals
- Aim for high protein foods such as chicken, fish, eggs, tofu and dairy products including milk and yoghurt.
- High energy foods such as full cream dairy, nut butters, avocados, bread/croissants, cheese etc especially if you are losing weight without trying.
- High nutritional supplements may be recommended if it is difficult to tolerate regular food
- Low fibre foods- especially if a flareup is causing a blockage or stricture (narrowing of the bowel)
- An intake lower in Fermentable carbohydrates may be able to assist in managing symptoms – a food and symptom diary would be helpful to record foods aggravating symptoms.
- Keep hydrated drinking at least 8 glasses of water a day.
Are there any foods I shouldn’t eat?
Certain foods may cause additional discomfort during a flare up. In those times it is important to listen to your body and avoid certain foods that irritate your gut. There is no need to avoid items containing gluten or dairy unless you have an intolerance to them. A low fibre diet may be recommended by your doctor or dietitian for a short period of time if you are experiencing a flare to help reduce symptoms like cramping
Always seek advice from a qualified health care practitioner; your doctor or dietitian, before making any significant changes to your diet.
What should I eat when the disease is not active or in remission?
- Follow a healthy balanced diet
- Eat from the five food groups (breads & cereals, meat & alternatives, dairy, fruit & vegetables).
- Consume at least 25g of fibre per day to keep your bowel healthy and regular.
- Aim for 8 cups of fluid per day.
- If still experiencing symptoms in remission, you may have food intolerances. Talk to your dietitian or health care practitioner.
Where can people go to find out more?
If you have noticed any of these symptoms or are concern that IBD may be affecting you, please visit your trusted GP. To learn more about these conditions and what life might be like for someone living with IBD visit:
Crohn’s & Colitis Australia or Support Australia
If you are wanting to learn more about the management of Inflammatory Bowel Disease, speaking to a professional like a dietitian is one of the best places to start. For more information book in to see our Dietitian, Jean-Mari Mouton.
See reception at your local Club Active or call 1300 258 250 to book in with Jean-Mari.

Jean-Mari specialises in a variety of conditions resulting from Inflammatory Bowel Disease and can assist you in managing your symptoms.
BURLEIGH, BUNDALL and MURWILLUMBAH // please contact to arrange a time.
TWEED // On-site every Thursday. Contact for an appointment.
PARKWOOD // On-site every Friday. Contact for an appointment.
Source: Crohn’s & Colitis Australia & Support Australia & Queensland Health
–
–
Author: Munpreet Dillon – Student Dietitian // Edited: Jean-Mari Mouton – Senior Dietitian